Continuing Education in Oregon for Updated Periodontal Classifications
PURCHASE COURSE
This course was published in the July 2022 issue and expires July 2025. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the features of the 2018 American Academy of Periodontology and European Federation of Periodontology periodontal classification system.
- Define appropriate treatments for periodontal disease based on the stages outlined in the classification system.
- List the varying stages of periodontal disease used in the classification system.
In 2017, the American Academy of Periodontology and European Federation of Periodontology held a world workshop to formulate an improved classification system for periodontal disease. In 2018, the findings were published in the Journal of Periodontology and Journal of Clinical Periodontology. 1 Since its publication, the 2018 classification has become the standard used to classify and describe periodontitis. However, its clinical application as a guide to the delivery of care has remained unclear. We recently published a paper describing "decision points" for periodontal therapy based on the new classification.2 The goal of these decision points is to assist clinicians in using the advanced features of the new classification system to help formulate effective treatment plans. The decision points also assist operators in evaluating the effectiveness of periodontal therapies, thus helping to determine when advanced therapies are needed. This also allows better planning for periodontal maintenance schedules.
The 2018 periodontal classification can be accessed in detail at https://sites.perio.org/wp-content/uploads/2019/08/Staging-and-Grading-Periodontitis.pdf. Table 1 outlines the essentials of the classification. In its simplest form, it can be summarized as Stage I being the earliest manifestation of periodontal disease, and then progressing through stages II and III to Stage IV, which is the most severe manifestation. The speed of disease progression is described as grade A through C, with Grade A representing slow progression and Grade C indicating rapid progression.
The grade of a case is extremely important in determining a patient's long-term prognosis, but grading requires more than a single evaluation. When patients are initially classified, they are graded as B until the passage of time permits a more accurate estimate of periodontal disease progression. If it is determined that a patient has rapidly progressing periodontal disease (Grade C), prompt referral to a periodontist is recommended. The full classification article referenced earlier should be reviewed for more information on determining the speed of disease progression and grade assignment.1 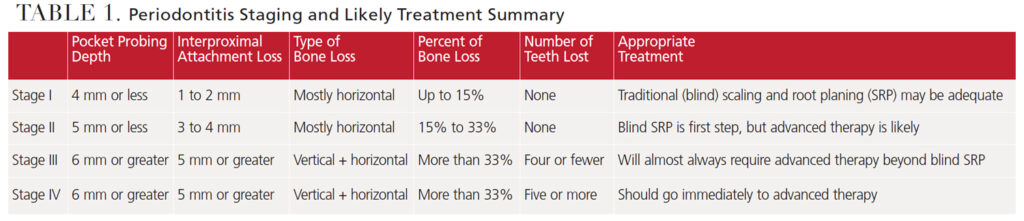
DEFINITIONS OF THERAPY
Self-Care Instruction: The need for patient education emphasizing the importance of meticulous self-care cannot be overemphasized. Not only does quality self-care help preserve oral health, it also facilitates ongoing diagnoses and disease management. Absent quality self-care, it is difficult to determine if a site that shows persistent signs of inflammation (e.g., bleeding on probing) is experiencing gingival or periodontal inflammation. This distinction can be important because gingivitis is easily addressed, whereas persistent periodontitis calls for additional periodontal instrumentation and, frequently, advanced periodontal therapy.
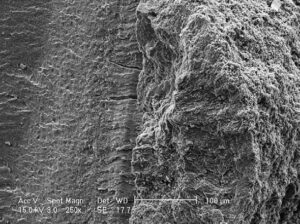
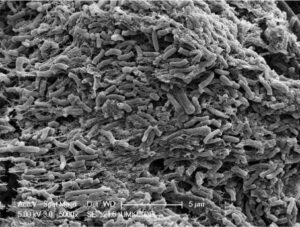
Scaling and Root Planing (SRP): This therapy removes calculus and roughness from the root surfaces of diseased (periodontally involved) teeth. Unfortunately, the removal of all calculus from the root surface can be difficult if the teeth have more than a few millimeters of periodontal pocketing. While bacterial plaque is the proximate cause of periodontal degeneration, once subgingival calculus has formed, it must be completely removed from the root for SRP to be a successful treatment for periodontal disease. So-called "disinfection of the root surface" (removal of subgingival surface plaque, but not subgingival calculus) is inadequate when subgingival calculus is present. Figure 1 and Figure 2 show that pathogens are harbored in residual calculus.
Research demonstrates that even sterile calculus is cytotoxic, meaning it kills periodontal cells.3 There are many clinical observations that residual calculus is present at sites that do not respond adequately to periodontal treatment. In addition, multiple studies have shown that skilled operators with unlimited operating time frequently leave a large percentage of undisturbed and fractured calculus on root surfaces following routine closed (i.e., blind) SRP.4 Additional research suggests that "microislands" of calculus remain after SRP, even with direct (open) visualization of the root surfaces. Thus, residual and fractured subgingival calculus remaining after SRP is undoubtedly a major cause of inadequate treatment of periodontitis.5
Advanced Therapy: Advanced periodontal therapy goes beyond traditional closed SRP, and may involve advanced visualization techniques, such as the use of a videoscope or periodontal endoscope, surgical access for (open) debridement of the periodontal lesion, and/or soft or hard tissue regenerative procedures. The type of advanced therapy used should be an informed, educated, and justifiable decision made by the therapist. Repeated unsuccessful closed SRP does not represent advanced therapy. If closed SRP does not resolve signs of periodontal inflammation, the patient should be informed of the need for, and availability of, advanced therapy.
Laser-based periodontal therapy is sometimes promoted as a stand-alone substitute for closed SRP or as an adjunct to traditional SRP. However, assessment of nearly 30 years of comparative studies suggests no additive benefit to lasers.6 Advanced therapy may be performed by any clinician who is adequately trained to legally perform such therapy. Nevertheless, advanced therapy necessitates a level of care equivalent to that expected from a fully trained periodontist.2
Reevaluation of Therapy: Reevaluation of the patient following all levels of periodontal therapy is mandatory in order to evaluate if the therapy has restored periodontal health. Depending on the treatment performed, patient reevaluation should occur at six weeks to three months post-therapy. If the patient returns to periodontal health after treatment, active therapy can be considered complete and the patient placed on a maintenance schedule.
Upon reevaluation, if the patient continues to have inflammation, bleeding on probing or deep pockets, the patient should be informed of the need for, and availability of, advanced care. Performing any level of periodontal therapy and not reevaluating the results and informing the patient of the availability of any necessary additional treatment or maintenance care, when appropriate, constitutes inadequate care.
Periodontal Maintenance: Periodontal disease is never completely cured, but it can be controlled. Patients who have been diagnosed with periodontal disease (Stage I through Stage IV) and adequately treated should always be placed on a schedule aimed at maintaining periodontal health. Seminal to proper maintenance care are routine reevaluations to determine if active periodontitis has returned. Patients who continue to show signs of active periodontitis (Stage I through Stage IV) should not be placed in periodontal maintenance, but, rather, should be provided advanced periodontal therapy.
CLASSIFICATION AND TREATMENT
Gingivitis: Gingivitis is not classified as a periodontal disease, but as gingival inflammation because pocket depth is not appreciably increased in gingivitis. The treatment for gingivitis is patient education and oral prophylaxis. By itself, SRP is not appropriate care for gingivitis. Studies have shown that SRP in shallow pockets can actually cause an increase of clinical attachment loss (CAL).7
Stage I Periodontitis: This stage of periodontitis is characterized by pocket depths ≤ 4 mm, clinical attachment loss of 1 to 2 mm, and/or radiographic bone loss ≤ 15%. Stage I treatment is usually performed by the primary practitioner following a nonsurgical protocol. Treatment typically consists of oral hygiene instruction, oral prophylaxis of pockets of 3 mm or less, SRP performed in deeper pockets, and site-by-site reevaluation and recording of responses to treatment (ideally at six weeks posttreatment). Assuming the patient adequately responds to therapy, he or she can be placed on a periodontal maintenance plan that may start at every three months, with a goal of six-month intervals. Complete periodontal reevaluation is necessary at each maintenance visit. If active disease recurs or progression of anatomic damage is noted, the patient should be returned to active therapy at the stage of periodontal disease presented at the time of reevaluation.
Stage II Periodontitis: This stage is characterized by pocket depths ≤ 5 mm, CAL of 3 to 4 mm, and/or radiographic (mostly horizontal) bone loss of between 15% and 33%. Limited furcation (class I) involvement may be noted.
Stage II treatment may be carried out by the primary practitioner, or the patient may be referred to a periodontist. The decision for referral will be based on a thorough evaluation of the patient's periodontal condition and practitioner's skill level. Stage II treatment usually consists of oral hygiene instruction, oral prophylaxis of pockets of 3 mm or less, SRP performed in 4 to 5 mm periodontal pockets, and reevaluation of response to treatment, ideally at six weeks posttreatment.
Assuming the response to therapy is adequate, the patient should be placed on a periodontal maintenance schedule. It should be noted that compared with Stage I cases, adequate response to closed SRP is less likely to occur in some Stage II cases. Many factors may be responsible, but the most frequent cause is the inadequate removal of all subgingival calculus and roughness using blind SRP. If the patient has not returned to periodontal health at the time of reevaluation, he or she should not be placed on a periodontal maintenance schedule; rather, active therapy should continue, with modifications to better address the unique nature of the circumstances. This might consist of further closed SRP, but advanced care is almost always indicated.
On the other hand, if the patient displays periodontal health, he or she should be placed on a three-month periodontal maintenance schedule, with reevaluation at each maintenance visit. If signs of active disease recur or progression of disease is noted, the patient should be returned to active therapy at the stage of periodontal disease presented at the time of reevaluation(s).
Stage III Periodontitis: This is an advanced stage of periodontal disease and will usually not fully respond to nonsurgical (i.e., SRP) therapy. Based on this, initial referral to a periodontist for advanced care should be considered. Stage III periodontitis is characterized by pocket depths ≥ 6 mm, CAL ≥ 5 mm, radiographic bone loss of more than 33%, multiple Class I to Class III furcation involvements, and/or loss of four or fewer teeth due to periodontal disease.
Stage III treatment will almost always necessitate the use of advanced periodontal therapy, which typically consists of:
- Oral hygiene instruction
- Exhaustive evaluation of risk factors (such as anatomic challenges or systemic medical concerns)
- Instrumentation (SRP), usually performed on all teeth
- Reevaluation of response to initial treatment (SRP) at six weeks
- Treatment planning for advanced therapy, including a prosthetic treatment plan if indicated
- Performing advanced therapy, which will frequently be surgical in nature and may include treatment to sculpt remaining tissue and/or regenerate lost tissue (bone and/or soft tissue)
- Placement on a periodontal maintenance and reevaluation schedule of every three months, depending on the response to therapy
More frequent maintenance visits may be indicated in some situations, with the goal of increasing the time between maintenance intervals if patient response permits. In all cases, if active disease returns or progression of disease is noted, the patient should be returned to active therapy at the stage of periodontal disease presented at the time of reevaluation.
Stage IV Periodontitis: This stage is characterized by periodontal tissue degeneration greater than would be expected, based on existing etiologic factors, such as the amount of plaque, calculus accumulation, age, and other risk factors. There may also be evidence of past rapidly occurring episodes of bone and attachment loss. Stage IV periodontitis will frequently present as multiple lost teeth and extensive prosthetic needs due to bite collapse and other factors. The periodontal conditions for Stage IV, such as pocket depth, CAL, furcation involvement, and other factors, are the same as in Stage III. The difference between the two is the extent of damage and loss of five or more teeth to periodontal disease.
Managing Stage IV periodontitis will require a team approach. Due to tooth loss and occlusal changes, prosthetic planning will always be part of therapy. Additionally, other disciplines — including orthodontics, endodontics and physician consultation — should be considered for the multidisciplinary team. The treatment of Stage IV periodontitis is usually best performed under the supervision of a periodontist. Advanced care is necessary for treatment of Stage IV cases and will vary with each patient. A specific description of therapy for Stage IV periodontitis is beyond the scope of this paper.
SUMMARY
Several studies report that many "hopeless" periodontally involved teeth are salvageable for extended periods with appropriate and timely therapy.8–11 The treatment recommendations presented here are based on our many years of private practice, and academic and public health experience. Therapy should always be individualized for each patient, so no single treatment approach is correct for all patients — or even for the same patient at different times.
In early cases of periodontitis (Stage I and possibly Stage II), basic treatments — such as oral hygiene instruction and SRP — may be adequate, but, in many cases, these treatments will not resolve the disease. This can only be determined by meticulous and frequent reevaluations that hopefully lead to appropriate modulations of subsequent care. Moreover, if periodontitis is not controlled by the treatment rendered, the patient must be informed of the need for, and availability of, advanced care. In closing, the repeated use of basic therapies — such as closed (blind) SRP — that fail to control periodontitis is neither adequate nor ethical.
References
- Caton JG, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri-implant diseases and conditions — introduction and key changes from the 1999 classification. J Periodontol. 2018;89(Suppl 1):S1–S8.
- Harrel SK, Cobb CM, Sottosanti JS, Sheldon LN, Rethman MP. Clinical decisions based on the 2018 classification of periodontal diseases. Compend Contin Educ Dent. 2020;43:52–56.
- Ziauddin SM, Alam MI, Mae M, et al. Cytotoxic effects of dental calculus particles and freeze-dried Aggregatibacter actinomycetemcomitans and Fusobacterium nucleatum on HSC-2 oral epithelial cells and THP-1 macrophages. J Periodontol. September 5, 2021. Online ahead of print.
- Caffesse RG, Sweeney PL, Smith BA. Scaling and root planing with and without periodontal flap surgery. J Clin Periodontol. 1986;13:105–210.
- Harrel SK, Wilson TG Jr., Tunnell JC, Stenberg WV. Laser identification of residual microislands of calculus and their removal with chelation. J Periodontol. 2020;91:1562–1568.
- Cobb CM. Lasers and the treatment of periodontitis: the essence and the noise. Periodontol 2000. 2017;75:205–295.
- Cobb CM. Nonsurgical periodontal therapy: mechanical. Annals Periodontol. 1996;1:443–490.
- Cobb CM, Sottosanti JS. A re-evaluation of scaling and root planing. J Periodontol. 2021;92:1370–1378.
- De Beule F, Alsaadi G, Peric M, Brecx M. Periodontal treatment and maintenance of molars affected with severe periodontitis (DPSI = 4): an up to 27-year retrospective study in a private practice. Quintessence Int. 2017;48:391–405.
- Díaz-Faes L, Guerrero A, Magán-Fernández A, Bravo M, Mesa F. Tooth loss and alveolar bone crest loss during supportive periodontal therapy in patients with generalized aggressive periodontitis: Retrospective study with follow-up of 8 to 15 years. J Clin Periodontol. 2016;43:1109–1115.
- Graetz C, Dörfer CE, Kahl M, et al. Retention of questionable and hopeless teeth in compliant patients treated for aggressive periodontitis. J Clin Periodontol. 2011;38:707–714.
FromDecisions in Dentistry. July 2022;8(7)26-29.
Source: https://decisionsindentistry.com/article/decision-points-periodontal-therapy/
Post a Comment for "Continuing Education in Oregon for Updated Periodontal Classifications"